Poxed and Abandoned
On May 13, the UK Health Security Agency reported two new cases of monkeypox in London, bringing the tally of recently identified cases of the heretofore rare disease—already endemic in West and Central Africa—to three. According to the agency, the new instances were entirely unrelated to the first, which had been identified in a recent visitor to Nigeria. This suggested that the virus was already spreading through the population, perhaps even globally. Indeed, ten days later, there were eighty suspected cases of monkeypox across a growing number of countries outside of Africa, including the United States, which identified its first case on May 18.
It would not, however, be until July 23, by which point just over sixteen thousand cases had been reported worldwide, that the World Health Organization (WHO) finally declared the situation a “public health emergency of international concern.” By then, some officials in the United States were already of the mind that the “window for getting control” of the outbreak had closed, even as the federal government dithered on whether to declare it a public health emergency, enabling a more coordinated response. It would take until August 4—seventy-eight days after the first case was identified in the States—before the Biden administration finally relented.
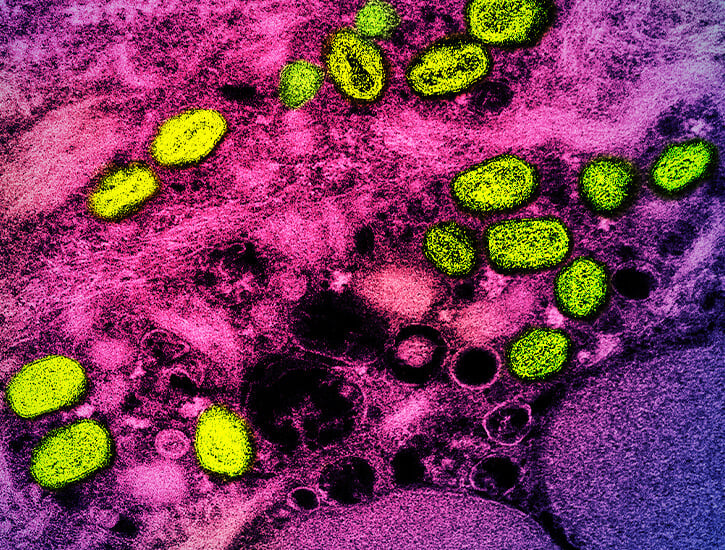
The slow and bungled response to the outbreak has not been due to a lack of available interventions. There is a vaccine available globally to prevent infection, distributed in the United States as Jynneos, which was initially developed to immunize against smallpox. Nations across the globe were unprepared for a worldwide outbreak, though, and are suffering from a shortfall of vaccines, with just one million doses available in early July. Accordingly, local and national health authorities have begun to prioritize access to the vaccine. Criteria differs from place to place but typically encapsulates known contacts of monkeypox cases and individuals at the highest risk of exposure—namely, men who have sex with men (MSM), especially those with multiple sexual partners. At the time of writing, 98 percent of monkeypox infections—characterized by fever, headache, swelling of the lymph nodes, and painful lesions across the body—have been identified in MSM, with 95 percent of infections suspected to have been spread through sexual activity, though the CDC indicates it can spread through other forms of “close personal contact.”
Anxieties abound that public discourse around monkeypox represents a grim resurgence of medico-moralizing about queer sex.
When Tedros Adhanom Ghebreyesus, the director-general of WHO, declared monkeypox to be a public health crisis, he urged nations to “work closely with communities of [MSM], to design and deliver effective information and services.” These measures have been met by criticism from a baying online public, apparently furious about the homophobic undertones of this messaging and the echoes of the conservative response to the AIDS crisis some four decades earlier. Indeed, there are echoes of AIDS-era homophobia in the global response to the monkeypox crisis, but these have been woefully misrecognized by the growing tide of public resentment, which all too often fails to name health authorities’ sluggishness as a problem in and of itself.
The backlash against public health messaging about monkeypox tends to fixate on the demarcation of MSM as an at-risk group. When WHO tweeted a transcript of Ghebreyesus’s statement, Twitter users were quick to point what they viewed as an apparent contradiction. “Why are you putting the emphasis on [MSM] when anyone can catch it via skin-to-skin contact, surface contact, airborne droplets exposure, etc.,” wrote one individual. “You’re literally creating AIDS 2.0.” Others posted images of homophobic tabloids from the 1980s characterizing the AIDS crisis as a “gay plague.” Writing in Mens Health, the journalist Philip Ellis expressed his disdain for press misrepresentations of monkeypox as a sexually transmitted infection spreading between MSM, suggesting that this echoed early framings of AIDS as a “gay” disease, “bolstered by the conservative idea that queer sex is dirty, shameful, and immoral, and that the people contracting HIV somehow deserved what happened to them.” Anxieties abound, then, that public discourse around monkeypox represents a grim resurgence of medico-moralizing about queer sex, positioning it as, in the words of Leo Bersani, not “merely increasing the risk of infection . . . [but] the sign of infection.”
These critiques can be divided into two rough, but interwoven, clades. In the first camp are those whose primary concern is about a rising tide of anti-gay sentiment that might accompany the demarcation of MSM as “high-risk.” Concerned about a conservative conflation of the medical and the moral that is bound to heighten scorn for queerness as a form of contagion, these critiques have tended to point out that MSM is an uncomfortably broad category, failing to distinguish between identity and behavior. These anxieties circulate, in particular, the labeling of all sex between men as “high-risk”—regardless of whether it is casual or coupled, monogamous or promiscuous—as well as the apparent danger of pointing out (even without judgement) that a certain proportion of queer men have plenty of it. For critics like Ellis, this failure of communication “can create a very real risk of violence.”
The second, related, set of critiques posit that positioning MSM as a demographic of concern shifts the focus of public health away from the spread of monkeypox in the wider population. The logic goes that the homophobic fixation on infection in queer men has siphoned the finite resources available—including vaccines and testing infrastructure—away from other demographics, particularly women and children, who remain at risk of monkeypox exposure by virtue of its modes of transmission.
But the MSM label was invented to address precisely some of these concerns. In the early years of the AIDS crisis, public health officials were searching for language that would help them address and serve men who did not necessarily identify as gay or bisexual but were otherwise at risk of HIV infection. The MSM label was also supported by those who were, according to the sociologist Gary Dowsett, in search of a “non-oppressive politics of HIV/AIDS,” offering an opportunity for public health messaging to focus upon risk practices rather than identities.
There is no doubt that MSM is an imperfect category. Taken alone, it cannot, as critics note, necessarily delineate who is at less or more risk within a network of MSM whose sex—itself an awfully vague term—varies in frequency and form. This, of course, is precisely why scarce monkeypox vaccines are largely being prioritized for MSM with multiple sexual partners, in recognition of the fact that not all risks within this cohort are equal; the risk of infection for a man who has sex with ten men in a week is exponentially greater than that of a man who has sex with one. Moreover, it also couches a judgement that the MSM sexual field is tightly bounded and discrete. As such, frequent close contacts of MSM who might not otherwise fit this label—including women (cis- and transgender) who have sex with MSM and non-binary people—may be neglected as subjects also requiring medical interventions.
But the current angst about the MSM category also marks a refusal to recognize and confront what we might call real risk: the fact that infection risk can be structured not only by the nature of behavior but also the identities that organize the way people socialize. Viruses, whether monkeypox or HIV, can spread selectively and disproportionately among groups like MSM not because of the questionable nature of their practices but because of the realities of their mingling. Queer men, for instance, coalesce more often and in close contact with other queer men at clubs, saunas, and apartments, as well as at parties and during hookups or dates. In this sense, identity and behavior may both contribute to infection risk. While this simple fact can be weaponized by conservative forces to depict a community as perverse or unclean, a virus makes no moral judgements. It is a wild, stochastic thing, caught in the bounds of an unlucky community and ricocheting again and again until it chances on a pore and breaks loose.
The aforementioned “anti-homophobic” critics have given primacy to paranoia about the social rather than the real risk posed to the queer community by monkeypox. This defensive position, unfortunately, threatens to exacerbate the conditions that conservatives might latch onto in the first place by discouraging health authorities from prioritizing interventions where they are most urgently needed. I see the importance given here to social risk above all else as consistent with a “post-AIDS” politics that defines much of the contemporary gay political landscape. I have previously identified such a politics behind efforts to overturn “gay blood bans” worldwide. These campaigners have taken aim at blood donor deferral criteria for homophobically labeling MSM as high-risk donors, expressing an eagerness to distance gay and bisexual men from the stigma of HIV infection and the image of queer men in the cultural imagination, which was crystallized during the AIDS crisis, as depraved silos of infection. Yet such a politics, which Rory Crath and Cristian Rangel have termed “performative cleansing,” comes at the expense of confronting an urgent reality. Namely, that MSM remain hundreds of times more likely than their heterosexual counterparts to seroconvert, with poor and Black MSM at the greatest risk of HIV infection.
This myopia lies at the heart of this current wave of public health criticism. Like many blood donor activists, critics of the MSM-first approach to monkeypox crisis have misrecognized the locus of homophobia, which lies not in the “singling out” of MSM as at-risk but in the reluctance to respond to monkeypox in the first place. Not only did WHO take well over two months to formally recognize it as a crisis, but reports of national vaccine management have revealed an inertia among public health officials to act with any urgency. For instance, the New York Times has reported that the U.S. government “adopted a wait-and-see” approach to the outbreak, allowing three hundred thousand vaccines to sit, unshipped, in a warehouse in Denmark, even as demand surged across the country.
It is this form of bigotry—manifest as state neglect—that allows viruses to spread, unchecked, among marginalized communities and that has historically structured the unequal pattern of epidemics. Notoriously, the Reagan administration’s response to the outbreak of AIDS crisis was one of cruel indifference: it wasn’t until 1985, by which point over five thousand people, most of whom were gay men, had died, that Reagan even deigned to mention the virus in public. Members of the activist group ACT UP New York, including Larry Kramer, began to compare the government’s handling of the spread of HIV to the Holocaust, framing it as, in the words of the sociologist Steven Epstein, a “genocide-by-neglect.” Contemporary critics suggest that in labeling MSM “high-risk” and naming them as priorities for care, public health authorities have symbolically condemned queer men as vectors of disease. The truth is, however, that by deprioritizing them, through a lackadaisical approach to those same interventions, whether motivated by disdain or apathy, health authorities have helped manifest epidemiological realities that mean queer men are at higher risk of certain infections.
It is what public health officials didn’t do, rather than what they did, that may have set the unequal foundations for the shape of monkeypox crisis to come.
Of course, sexuality is not the only axis along which neglect may be enacted: race and class are key determinants of health care provision. Activists in the UK have expressed concern over the current modes through which scarce vaccines are being provided. Will Nutland, cofounder of the grassroots sexual health campaign PrEPster, has noted that “‘free-for-all’ super-vax events over-serve people who can queue for hours, who don’t have care responsibilities, who don’t have a weekend job to work, or who are OK being spotted in a ‘gay’ queue,” and points out that this means “they are less likely to serve Black and brown queers.” First-come first-served vaccine appointment systems will also prioritize those with the most flexible schedules and, therefore, will be unlikely to cater to those with, for example, zero-hour contracts. Unsurprisingly, data already suggests that Black and Hispanic MSM are shouldering a disproportionate burden of monkeypox infections.
More broadly, the current outbreak of monkeypox across Europe and North America can be explained by a sustained and racially motivated indifference toward disease in Africa. Scientists have harshly condemned nations in the Global North for ignoring outbreaks of monkeypox in Central and Western Africa that have been reported since 1970, most recently in Nigeria from 2017 to 2019. Speaking to Nature, Adesola Yinka-Ogunleye, an epidemiologist from the Nigeria Center for Disease Control, opined that “the world is paying the price for not having responded adequately” to recent monkeypox outbreaks. Just as the spread of monkeypox in the West may have been ignored because of a latent regard for queer men as inherent disease risks, it has gone overlooked in the Africa for decades thanks to the colonist’s view that, as the philosopher Arianne Shahvisi suggests, explains and naturalizes “the disease-prevalence of ‘tropical’ regions by reference to [the environment], rather than colonialism and neocolonialism.”
There is a bitter irony, then, that current, allegedly anti-homophobic, criticisms of public health interventions include claims that by prioritizing MSM, officials are neglecting a wider population. Nothing could be further from the truth: it is no coincidence that the WHO declared monkeypox to be an emergency only after cases of the virus began to be identified within children. Certainly, and according to Anthony Fauci, monkeypox may pose a greater risk of harm to vulnerable groups like children—but the abrupt hysteria of media outlets and public health officials alike is indicative of a blatant devaluing of queer life in the West, redolent of the moment when, in 1983, reports of cases of AIDS among infant blood transfusion recipients caused tabloid hysteria that “innocent” heterosexuals might become infected with the virus that would come to be known as HIV. In kind, even in the context of a very different viral moment, with different routes of transmission and available interventions, a similar structure of heterosexual self-interest abounds. Anxieties about monkeypox apparently detected in the wastewater outside of San Francisco and on college campuses can shift the gaze of concern from an affected queer community to a speculatively affected heterosexual one.
This abysmal year has delivered us yet another global public health emergency in the form of monkeypox. And like the Covid-19 pandemic alongside it, it calls forth “lessons” to be remembered from the past and present of the AIDS crisis. Yet these attempts at pedagogy, cast out from an increasingly “pro-gay” public, have been severely misguided—taking aim at the one thing public health officials may have got right this time: an eventual attentiveness to the plight of queer men. It is what public health officials didn’t do, rather than what they did, that may have set the unequal foundations for the shape of monkeypox crisis to come. After all, what AIDS history, as well as the ongoing neglect of AIDS in the Global South, reveals is that the locus of homophobia—and other ills and isms—lies not in the terms of action but inaction.